Submit claims to Desjardins
Note: You'll need to create a Desjardins plan member account before you can submit a claim. Learn how to create a Desjardins Group insurance account.
This article will review how to:
Check if you have coverage from Desjardins
Submit insurance claims online through web or mobile
View claims status
Submit paper claims
Getting Started
Checking for Desjardins coverage
To check if your employer has Desjardins benefits through League, navigate to your League Wallet. You'll see a list of benefits. Clicking or tapping on a benefit will reveal more information. If you have Desjardins coverage, you'll see one or more benefit cards containing a Desjardins insurance logo:
For more information on your Desjardins policy, please refer to your Desjardins benefits booklet. This can be found in the League platform by:
Selecting a Desjardins benefit.
Navigating to “Actions”.
Selecting “Full Coverage Booklet”.
You can also access your booklet by contacting your employer, chatting directly to our Customer Care team through League in the "Chat" tab, or by sending an email to help@league.com.
When to submit claims to Desjardins
Desjardins is your insurance provider through your League benefits and:
If Desjardins is your primary insurer, all eligible insurance claims must be submitted to them first
Once Desjardins adjudicates your claim or makes a payment for an eligible item/service, you can "coordinate benefits " by submitting remaining expenses to any other insurance providers (such as your spouse's insurance coverage, etc).
If you have supplementary benefits with League, such as a Health or Lifestyle Spending Account, you can submit claims to League after all other forms of insurance have been applied . This helps maximize your coverage.
When you have Desjardins coverage, you'll have one or more of the following benefit cards in your Wallet:
Drug |
|
Dental |
|
Paramedical Services |
|
Medical Services & Supplies |
|
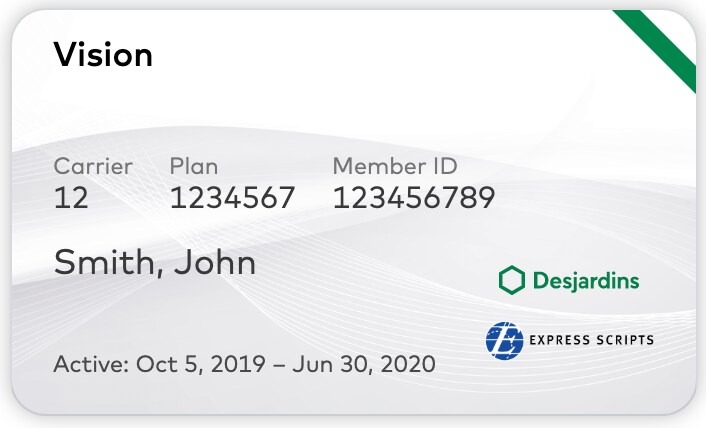
Vision |
|
For all other claim types, select the benefit that best describes the type of expense and follow the instructions under the "Overview" section.
Submitting claims to Desjardins
With Desjardins' plan member portal, you’re able to:
Submit claims electronically
Check claims status
Monitor your benefits coverage balances
Set up direct deposit for claim payments
To submit claims on the Desjardins plan member portal, log in to your account:
On web: Open the Desjardins web login page.
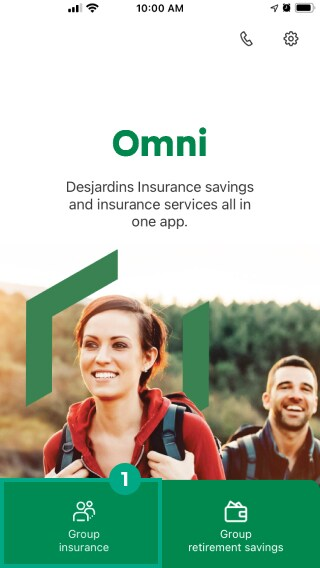
On mobile: Open the Omni app on your compatible smartphone or mobile device.
You can also access the web login page through your League account. Simply sign in to League > Navigate to your Digital Wallet > Select any of your Desjardins benefits > Click "Submit Claim via Desjardins".
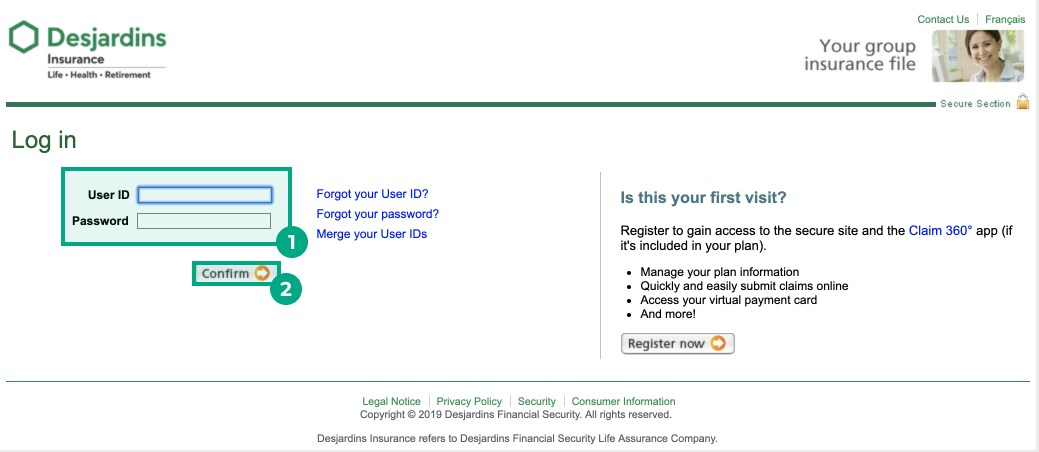
On web
1. Enter your User ID and password.
Note: If you haven't registered for Desjardins yet, see Create a Desjardins Group Insurance account.
2. Click “Confirm”.
You’ll now be logged in to your Desjardins plan member account.
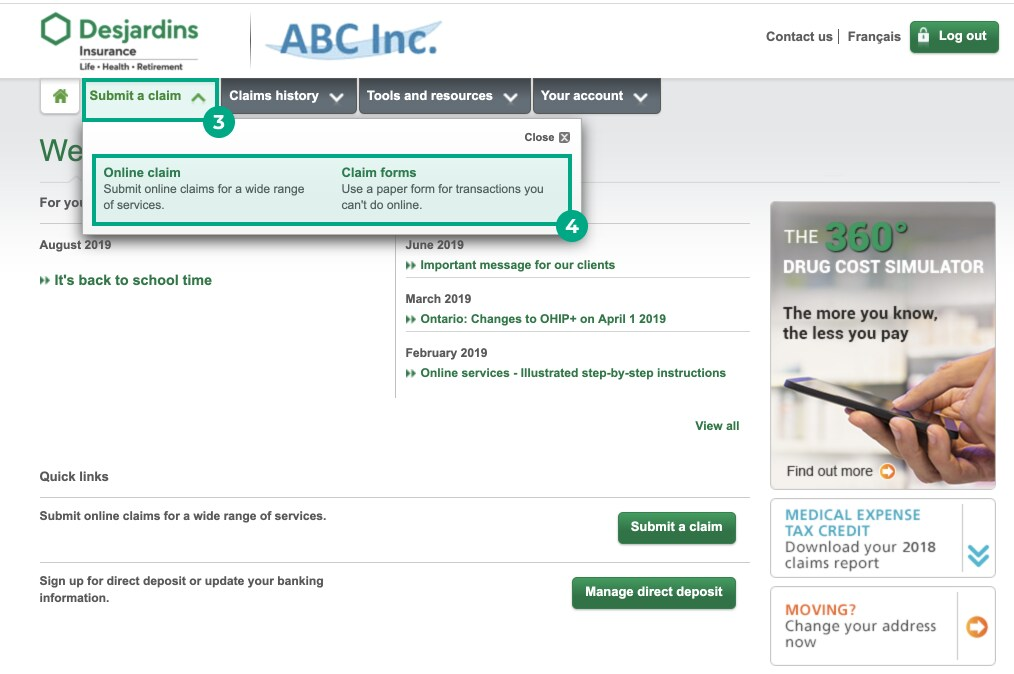
3. Click the “Submit a claim” tab.
4. Select either:
Online Claim (Continue to Step 5)
Paper Claim (Continue to Paper Claims section at the end of this article)
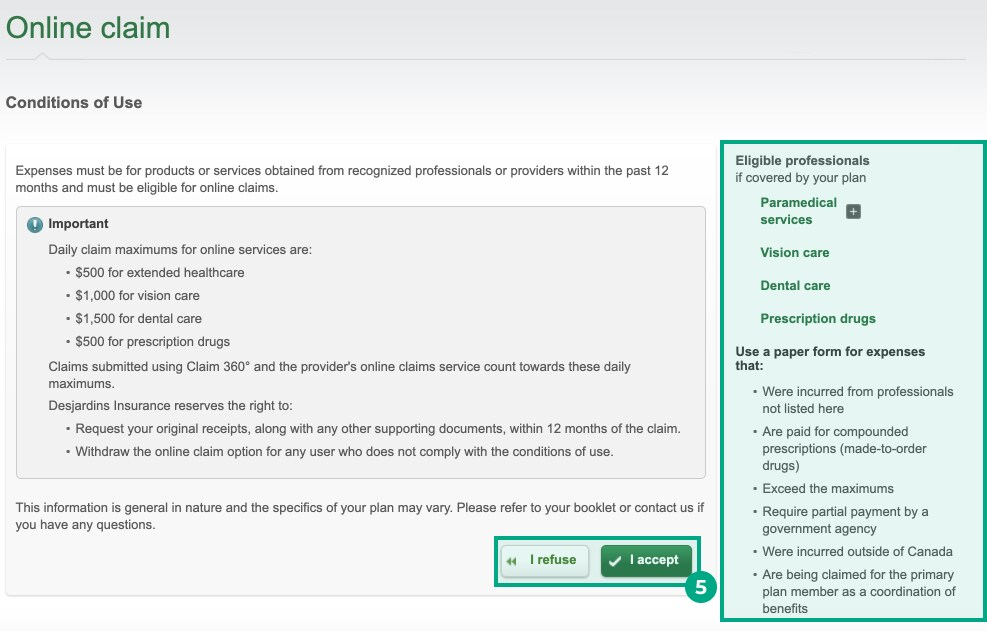
5. Read the Conditions of Use and click “I Accept” or “I Refuse”.
Note: Desjardins provides useful information on what professionals are eligible for submitting claims online, to the right of this page.
6. Select the name of the patient who received the service or treatment from the “Patient” drop-down menu.
7. Select the provider who provided the service or treatment from the “Provider” drop-down menu.
Note: If the provider isn’t on the list, click “Add/Edit” and fill out their information.
8. Fill out the following sections:
General Information (if applicable);
Prescription details (if applicable);
Service/Treatment/Drug details;
Calculation of amount claimed;
Additional information (if applicable).
9. Click “Add to Claim”.
Note: You can submit one claim for multiple expenses. After you finish adding the information for one claim and select “Add to Claim”, you can then use the same form to submit another claim.
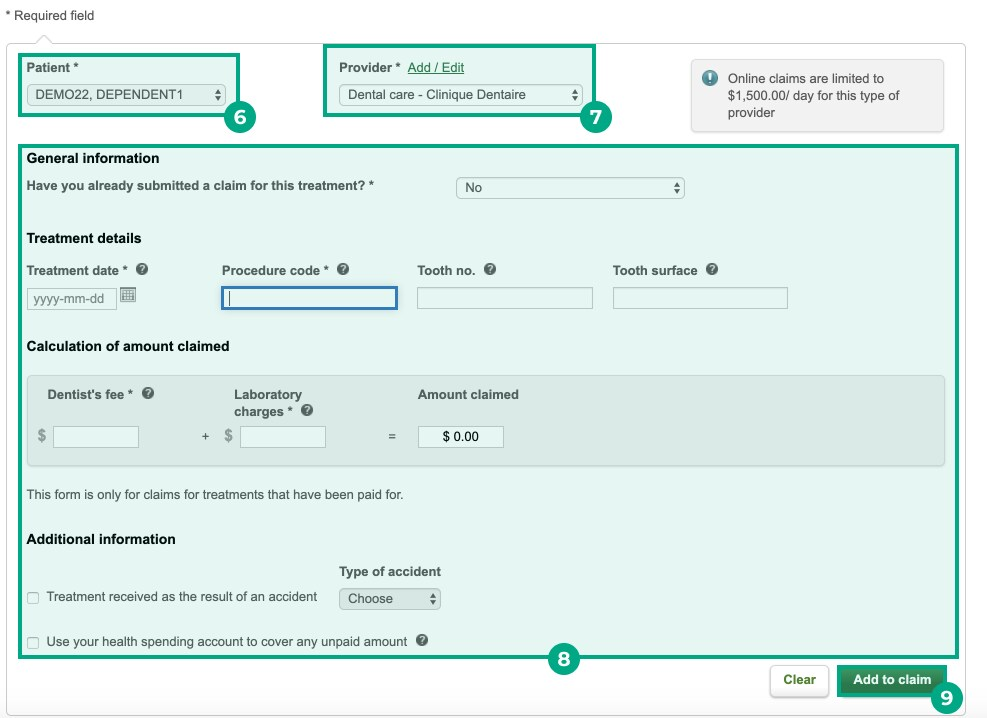
10. Click “Next”.
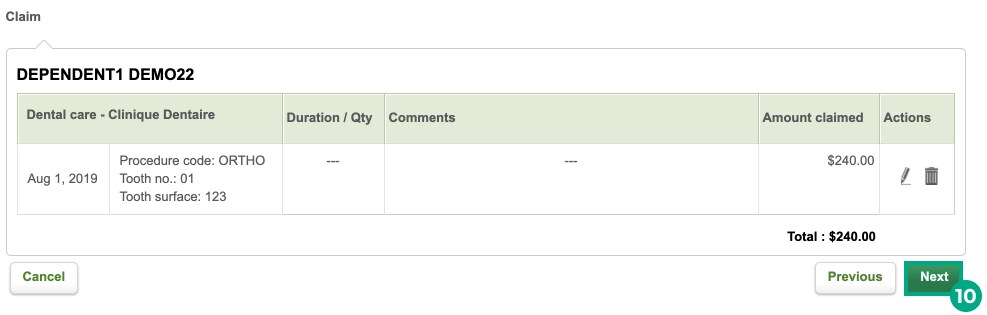
You’ll be directed to a confirmation page with the claim details. Your claim has been submitted!
On mobile:
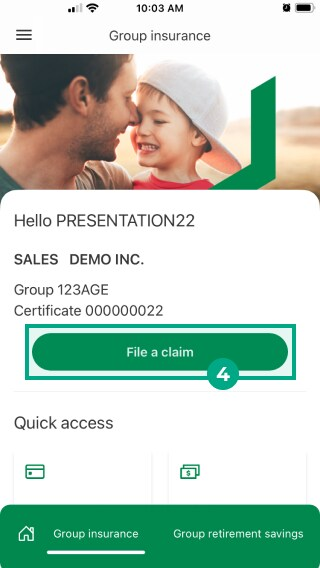
1. Open the Omni app and select “Group Insurance”.
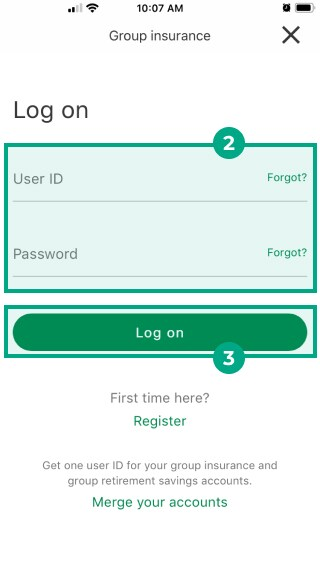
2. Enter your User ID and Password.
3. Click "Log on".
4. Click “File a claim”.
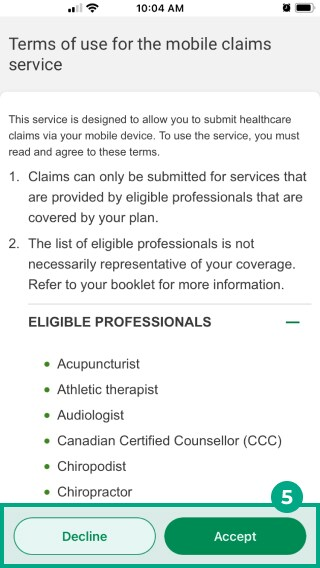
5. Read the terms of service for mobile claims service and tap "Accept" or '"Decline".
Note: Desjardins provides useful information on this page on eligible professionals for submitting claims via mobile.
6. Select the name of the patient who received the service or treatment under the “Patient” section.
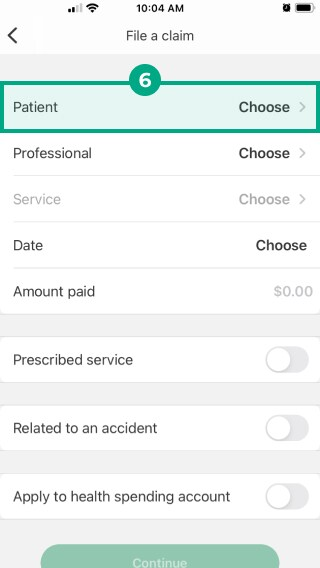
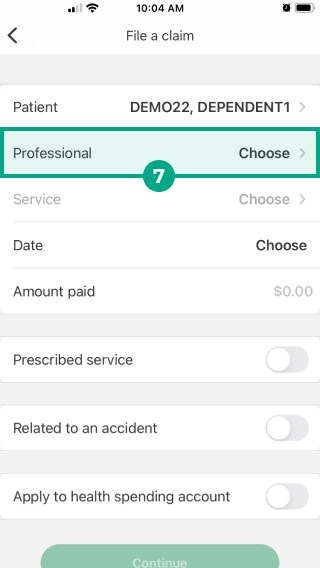
7. Select the healthcare provider who provided the service or treatment under the “Professional” section.
Note: If the name of the provider isn’t on the list, click the “+” symbol under the “Professional” section and fill in their information.
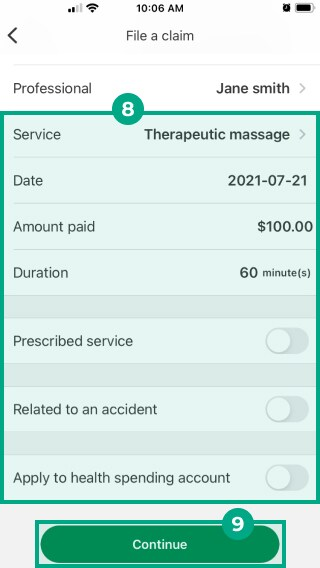
8. Fill out the following information:
Service;
Date;
Amount Paid;
Any additional information (if applicable).
9. Click “Continue”.
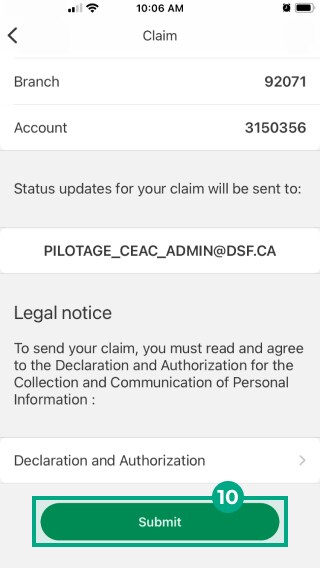
10. Review your direct deposit and contact information. If everything looks correct, click "Submit".
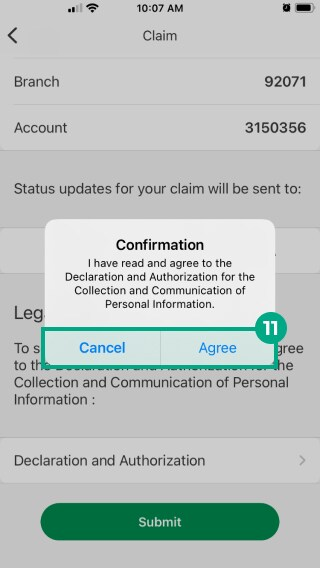
11. Read the Declaration and Authorization for the Collection and Communication of Personal Information, and select “Agree” or “Cancel”.
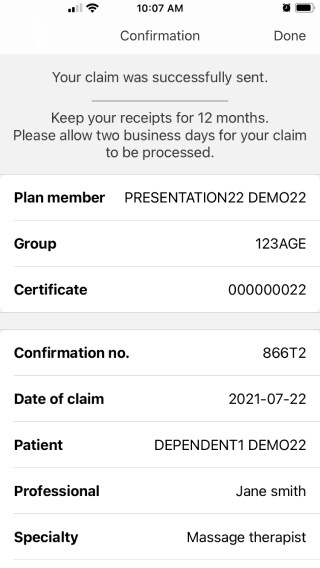
You’ll be directed to a confirmation page with the claim details. Your claim has been submitted!
Claim Status and Claim Forms
To check the status of your claim:
On Web |
|
On Mobile |
|
Most claims can be submitted online via the process described in this article, but some claims must be submitted to Desjardins with a paper form.
See a list of claims that are eligible for online or mobile submission (on page 5). If your claim isn’t on the list, you need to complete a paper claim form. Claims also can’t be submitted online if they:
Were incurred from professionals not listed in the document above
Are paid for compounded prescriptions (made-to-order drugs)
Exceed the maximums
Require partial payment by a government agency
Were incurred outside of Canada
Are being claimed for the primary plan member as a coordination of benefits
You can access a list of paper claim forms from your Desjardins online account (on web only) by clicking “Submit a claim” and selecting “Claim forms”.
Contacting Desjardins
Desjardin's contact number is: +1 (800) 263-1810
You can contact Desjardins from Monday-Friday, 8 a.m. - 5 p.m.
.png)